470,000 Bhutanese have to be infected and recover to achieve herd immunity: TAG
Younten Tshedup
When and how will the Covid-19 pandemic end?
While this has been the biggest question since the beginning of the pandemic earlier this year, epidemiologically, it was already known from the beginning how the end would arrive.
All pandemic ends when the pathogen runs out of people to infect or when it reaches a stage where the pathogen can no longer find enough susceptible hosts to survive (infect).
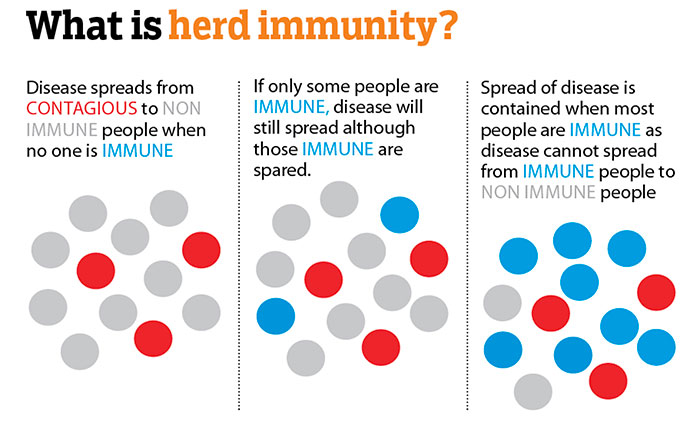
When enough people in a population become immune to a disease (in this case, Covid-19), the active chain of transmission is broken. As more people become immune, those infected are less able to pass on the disease, and the spread of the disease slows down. This is when a community, country or a population achieves herd immunity.
Dr Sonam Wangchuk, a member of the health ministry’s technical advisory group (TAG) said that herd immunity can be achieved through two means.
People can develop resistance to the virus naturally when the body is exposed and infected with the virus. The body produces antibodies to fight the infection. These antibodies remain in the person’s body and protect the individual from a re-infection.
When enough people develop the resistance in a community, it leads to herd immunity in the community.
Another way to achieve herd immunity is through vaccines, said Dr Sonam Wangchuk. A vaccine is usually composed of a fragment of the actual virus that triggers an immune response in the body when introduced. So, when a person is exposed to the actual virus, the body already has the antibodies ready to fight the infection.
When a community achieves herd immunity, it doesn’t mean that there would be no more infections. There will be sporadic cases, said Dr Sonam Wangchuk. However, he said that the transmission and spread is cut off as every third person in the community has immunity.
However, in absence of a vaccine for Covid-19, herd immunity for now could only be achieved if enough people contract the disease and recover, developing an immunity to it in the process.
However, achieving herd immunity is easier said than done. Experts say that a large number of populations would have to be infected if a community or country has to achieve herd immunity.
The US, with the leading positive cases currently has only about three percent of its entire population infected with Covid-19 currently. Experts say besides taking a long time, achieving herd immunity naturally would come at a terrible cost.
When does a population achieve herd immunity?
Dr Sonam Wangchuk said that to reach herd immunity, the threshold population – the minimum number of people with resistance to the infection – has to be reached first. And this depends on the type of virus and its reproduction rate (R0, read R-naught). The more contagious the pathogen (high R0), higher the threshold for herd immunity would be.
He said that considering the R0 of Covid-19 to be three, to control the spread of the infection and break the chain of transmission, at least 65 percent of the Bhutanese population had to be either infected or vaccinated. This would mean that more than 470,000 Bhutanese have to be infected and recover from the disease to achieve herd immunity.
However, he said that currently there are no clear findings that establishes the antibodies produced against SARS-CoV-2, the virus that causes Covid-19, provide long-term immunity against the disease. In other words, there is no guarantee that a person cannot get reinfected with Covid-19 once he or she has recovered.
He said that some of the scientific papers claimed that antibodies developed in a recovered Covid-19 patient provided protection for four months, while some claimed for a year. “SARS-CoV-2 is an unstable virus because it is an RNA virus. It changes frequently, which is why developing a lifelong immunity against the virus is not possible.”
The TAG team is planning to conduct a study among Bhutanese who had recovered from Covid-19 to see if they were still susceptible to a reinfection.
“This kind of studies has not been conducted widely and we want to see if these recovered people have enough antibodies to protect from a reinfection,” said Dr Sonma Wangchuk.
For this he said that samples from the recovered individuals would be collected to quantify the number of antibodies in their bodies. “But to conduct the study, we don’t have the machine that quantifies the antibodies. We only have the test kits that detect the presence of the antibodies for now.”
Vaccines
Considering the herd immunity concept, after an effective vaccine is developed, at least 65 percent of the population has to be vaccinated to control and break the chain of transmission in the country. Higher the vaccine coverage, the more effectively the spread of the disease would be contained.
Dr Sonam Wangchuk said that the dosage of the vaccine and its effectiveness on individuals is yet to be known. However, he said that even after a vaccine is produced, it would not mean Covid-19 would no longer be a threat.
Internationally, there have been indications that this may be like the flu, and that immunity may not last longer than four or five months. Meaning, that the immunity from the vaccine may wane over time, and people would need to be revaccinated.
This, however, is yet to be established.
Dr Sonam Wangchuk said that for flu, people receive vaccinations every year to be protected. He said that the protection is estimated to only be between 30 and 80 percent effective against whichever strains of flu virus that are circulating that season.
“This is a relatively new virus. For us to understand its nature, it has to be there in the population for a few years.”

